The Leapfrog Value-Based Purchasing (VBP) Program helps health plans, employers, and other purchasers identify the highest value hospitals in individual markets and across the country, based on the results of Leapfrog’s Hospital Survey.
Leapfrog applies its VBP Program methodology to Survey Results and gives each facility an overall VBP Value Score. The VBP Value Score can be used to rank the hospitals and set benchmarks for financial awards or incentives, such as awarding the highest reimbursement rate to hospitals scoring in the top decile. Performance can also be assessed by domain, such as maternity care or medication safety, and by measure, such as C-section rate or hand hygiene performance.
In the following interview, Leapfrog’s Director of Employer and Payor Engagement, Jill Berger, has a discussion with Michelle Merchant, Hospital Network Relations at Horizon Blue Cross Blue Shield of New Jersey, about their health plan’s journey using the Leapfrog VBP Program to spark improvement in the safety and quality of care provided by hospitals in their state.
Jill: Michelle, thank you for joining me today. Horizon has been one of our longest partners in using the Leapfrog VBP Program and has been using data from the Leapfrog Hospital Survey since 2006.
Michelle: Thank you, Jill. That is correct.
Jill: Michelle, you are one of the early adopters of using Leapfrog data in pay-for-performance programs. Can you talk about this and explain how it’s been beneficial to both your health plan and for all of New Jersey?
Michelle: As you mentioned, we've partnered with Leapfrog since 2006. Without a doubt, the partnership has been quite beneficial to Horizon members as well as the people of New Jersey in terms of their health care outcomes.
We started on this to provide incentives to our network hospitals for them to focus on improving health care outcomes. We were glad to partner with Leapfrog because the Leapfrog Hospital Survey is so good for benchmarking and tracking data, because hospitals were already engaged, and of course, because purchasers of health insurance and our services are behind the Leapfrog effort.
Jill: What's really impressive is that all but one hospital in New Jersey participates in the Leapfrog Hospital Survey, and for a while, 100 percent of hospitals participated. How has this high participation impacted the quality of inpatient care in New Jersey?
Michelle: From the beginning, our goal was always to get 100 percent of our network hospitals to complete the Survey. When we first started in 2006, only eight New Jersey hospitals completed the Survey. Based partly on the financial incentive we offered, more and more hospitals got on board.
We have also partnered with other stakeholders in the state, like the New Jersey Health Care Quality Institute - the local Regional Leader for Leapfrog - who have also strongly encouraged hospital CEOs to complete the Survey annually. We’re pleased to partner with and support the efforts of this important organization.
In 2019, we were pleased to achieve 100 percent participation in our state for the first time. The COVID-19 Pandemic changed things a little bit. Right now, we have only one New Jersey hospital that does not complete the Leapfrog Hospital Survey, though they’ve committed to us that they’ll submit their Survey before the deadline this year. We are confident that we’ll be back to 100 percent participation soon.
Jill: I know that one of the major domains in our Hospital Survey that you're focusing on is maternity care. Can you tell me more about this work?
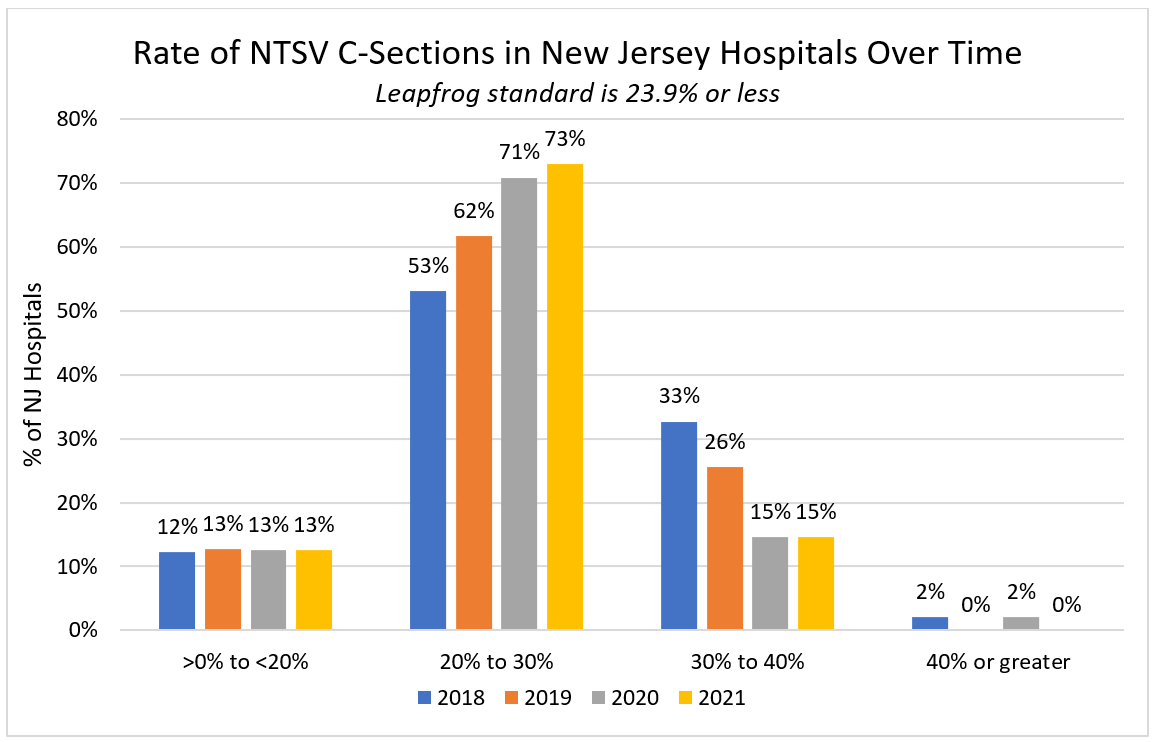
Michelle: We’re very proud of what we've done with maternity care – a very important issue in New Jersey. We were one of the early plan advocates encouraging the inclusion of the maternity care domain in the Leapfrog VBP Program. We became very invested in hospital performance around maternity care because the volume of hospital maternity care claims exceeds all other hospital claim submission categories. We were not only concerned about the safety of maternity services, but we were also alarmed that New Jersey was an outlier in terms of C-Section rates among all states.
The expected C-Section rate should be a little less than a quarter of all deliveries, but many New Jersey hospitals had a much higher rate, some twice as high as the national average. In some hospitals, the majority of their deliveries were C-sections. This was not good for our members or the population of New Jersey. We all know that C-Sections are necessary at times, but the majority of hospital deliveries should be vaginal births.
With the Department of Health and the New Jersey Hospital Association, we focused on C-Section rates as one of the earliest metrics we looked to address. We also introduced a Horizon Episodes of Care Program for Maternity Services, as part of a suite of value-based programs with our providers. C-Section rates were a key metric used in that program. What gets measured, gets managed. We were pleased at the improvements we saw.
In 2015, only 10 percent of our hospitals were performing C-Sections at a rate of 0 – 20% of total deliveries. 33% of our hospitals were performing C-Sections at a rate of 40 percent and higher - almost twice the national average. By 2018, the hospitals that had previously had a rate of 40 percent C-Sections, had reduced those numbers to 18%.
How did we get there? In addition to other efforts, we started providing educational programs for hospitals. Part of this education effort was to simply allow hospitals doing well to share and discuss the programs and best practices that were working well for them with all NJ hospitals.
For example, one hospital talked about its laborist program, which helped reduce pressure on obstetricians who lose valuable office hours when they need to check on laboring patients in the hospital. By having laborists on the team, in-house obstetricians who communicate with the patient's primary OB on their progress, primary OBs can better manage their time and know when they need to be at the hospital for delivery.
Jill: That is amazing progress. How did you encourage the hospitals to focus on improving C-Section rates and prioritizing transparency aside from payment incentives?
Michelle: For a good ten years we provided hospitals with a payment incentive. It was a very small incentive and payment incentives can only go so far but it did get the attention of hospitals and got things rolling in the right direction. In New Jersey, in line with national trends, we’ve seen fewer solo community hospitals and an increase in large, consolidated hospital systems. Cumulatively, for hospital systems, the incentive was a lot of money, but overall, it generally wasn’t a huge number.
Our collaborative efforts with Leapfrog and the New Jersey Hospital Association also played a large role in encouraging hospitals to “care” about maternity care quality and safety, including C-Section rates. The release of the performance data got attention. Hospital CEOs were being called upon to justify, defend and explain why they had such high C-Section rates. This was a good call to action to change. Since we had already started the work, the hospital quality directors were already engaged in it and knew it was a priority we all shared.
Jill: That's great. You mentioned that you have educational programs that you put in place for the hospitals. Can you tell me more about that?
Michelle: We usually get the benchmarking reports from Leapfrog (which hospitals also receive) around February or March of each year. Shortly after that, I convene a conference and invite representatives from all New Jersey hospitals. The conferences include presentations from Leapfrog. Their reports help us see where New Jersey hospitals are not doing well and provide a roadmap for what domains are a priority for us to focus on. The conferences allow us to publicly recognize hospitals whose reports reflect very good performance.
Most of the hospital quality directors are clinicians and nurses, who are used to and benefit from peer education, so we always include presentations by hospitals that have demonstrated success on a particular metric or domain. While reviewing mid-year reports, I reach out to hospitals whose reports look very good. I ask them what areas they have really worked on and if they have a story to share. I look at their performance and seek help from the high performers to educate and encourage those hospitals, who may not be as strong in certain areas, to get better.
We also invite experts to these meetings. For instance, we’ve had perinatologists come and talk about the dangers of C-Sections, especially early elective C-Sections, and the impact to the mother and to the infant. We archive these conference presentations and continue to share them as new people join the quality departments at NJ hospitals.
We never approach the review of metrics with hospitals in a punitive way. It's all about education and providing hospitals with resources to aid in improvements. We know that health care providers really want to make a difference and to do well.
Jill: This shows the importance of transparency and sharing best practices among peers. That is truly a success story. What advice do you have for other plans that are interested in starting a pay for performance program?
Michelle: I am a strong believer in partnerships between health plans and their providers. Hospitals are a vital part of that partnership and I believe that the Leapfrog Hospital Survey is a proven and effective method upon which to base a pay-for-performance program. It is a plug-and-play type of offering that Leapfrog provides.
I think it's worth it and I think when you have good outcomes and you do the right thing, patients benefit from it, and it helps the bottom line. Focusing on quality and improvements helps to attract new patients and new staff. It helps the health plans to minimize the costs of unnecessary care. For example, the cost difference between a C-Section and a vaginal delivery is vast, and in some health plans, it's a very significant difference. You also want to make sure that your members, the patients, are receiving the best care. Not to say a C-Section is never appropriate. There is a time and place for everything, and we want to make sure that care is being administered appropriately. I believe that providing financial incentives make a difference, especially at the beginning of a program, but it is not something that may be permanently necessary.
Hospital executives recognize that better outcomes are better business. We’ve seen the benefits of our pay for performance programs in New Jersey, and our First Lady, Tammy Murphy, has made maternity care outcomes a big part of her platform. This has really galvanized our efforts throughout the State.
Jill: Maternity care is a great place to start to make change. I can't agree with you more, Michelle. Thank you for speaking with me today and for sharing Horizon's incredible efforts. Thank you for what you do and for Horizon's commitment to the safety of your members and the community.
Michelle: Thank you so much, Jill. It’s really been a pleasure talking with you about one of the most gratifying aspects of my career and tenure at Horizon. One of the unexpected things that came out of these efforts and partnerships is that our hospitals came to see our health plan as an early champion of improving performance - never taking a punitive approach, but one of rewarding and recognition of quality improvements. And you know that's a priceless benefit and it's one that I believe will endure. Our partnership with Leapfrog has certainly made that very easy.